
Health insurance isn’t working for Americans like it should, particularly for Black Americans.
Commissioned by PhRMA and conducted by Ipsos in 2023, the latest Patient Experience Survey compiled the testimony of 5,000 insured Americans, representing a nationally representative sample, with results indicating that patient health care costs—including high premiums and deductibles, and ongoing out-of-pocket costs related to monthly prescriptions, doctors’ visits, and other health care services—create significant barriers for underserved individuals seeking basic healthcare or treatment of any unforeseen health emergencies.
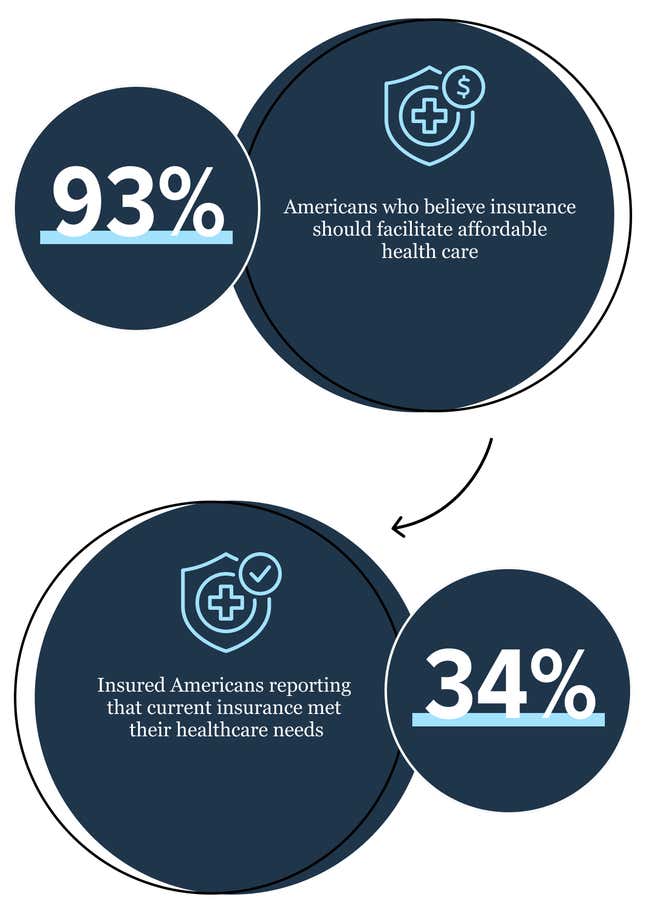
Among the survey’s sample, only 34% of respondents reported that health insurance currently provides everyone with affordable access to health care when it’s needed, with approximately 1 in 5 people (19%) saying their out-of-pocket healthcare costs would become unaffordable if they had a major unexpected medical event.
For Black communities, access to reliable, affordable healthcare is imperative.
Historically, structural racism and discrimination have driven inequities in access to health care. As a result, Black communities are more likely to experience life-threatening, unexpected health emergencies and chronic diseases than white people.
According to the Department of Health and Human Services’ Office of Minority Health, Black people have a higher likelihood of dying from many diseases, such as diabetes, heart disease, and prostate cancer, as compared to white people.
Black patients also report high levels of difficulty making the most out of their healthcare. For example, access to prescription medicine is curtailed for communities of color due to out-of-pocket costs from insurance and social and economic barriers. Researchers at the University of Southern California found that Black and Latino urban neighborhoods are more likely to be affected by pharmacy deserts than other urban neighborhoods. On average, in more than 40% of US counties, people are required to drive at least 15 minutes to reach a nearby pharmacy.
Read on for three key insights from PhRMA’s Patient Experience Survey underscoring the systemic barriers between Black Americans and their health.
Patient Insight #1
Affordability of basic out-of-pocket costs is a concern
Among insured Black Americans in PhRMA’s Patient Experience Survey, 64% expressed concerns about affording their copays, deductibles, coinsurance, and out-of-network fees.
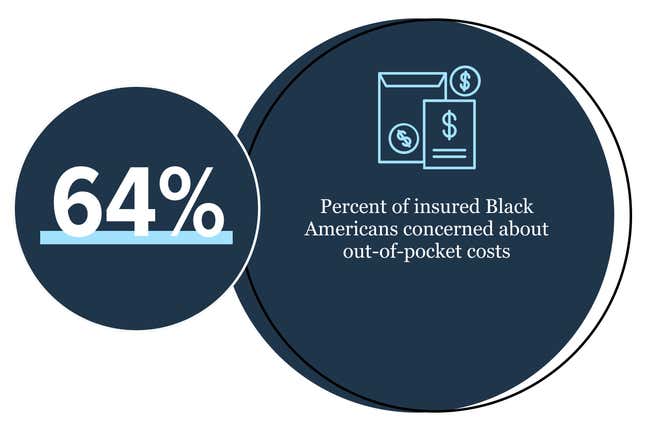
Even among the general population, out-of-pocket costs (like sky-high deductibles) are identified as the primary healthcare affordability issue, followed by steep premiums, and inefficiency in the healthcare system, including roadblocks like prior authorization for prescription medicines.
Whether or not the people seeking medical treatment can afford their doctor-recommended regimens, many have little to no choice to alleviate a health issue. Sometimes the care is even lifesaving.
This leads many to take on crushing amounts of medical debt—with the three biggest sources coming from hospital bills, doctor bills, and diagnostic tests. In fact, 1 in 4 insured Black Americans (25%) in the Patient Experience Survey reported outstanding medical debt, as compared to 1 in 6 insured white Americans (15%).
Patient Insight #2
Prescription costs are a serious pain point
Whether it’s insulin, an inhaler, or an antibiotic, millions of Americans rely on one-time or recurring doses of prescription medicine to manage chronic or acute medical conditions. According to the Patient Experience Survey, 98% of insured Americans value the portability and ease of taking a medicine in pill form purchased at their local pharmacy.
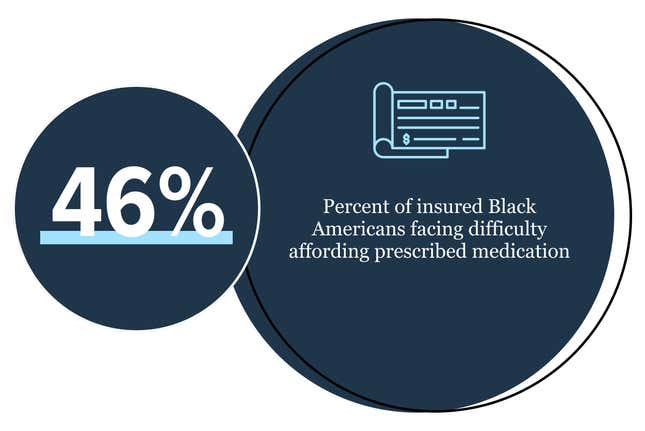
In the Patient Experience Survey, a staggering 46% of insured Black Americans expressed concern about being able to afford their prescription medication, compared to 38% of insured white Americans. Standard practices of pharmaceutical middlemen regularly prevent or delay Americans from receiving these life-saving treatments.
It’s often not the doctors determining what medications patients can access, but the pharmacy benefit managers (PBMs), who work on behalf of health insurers and the government, who are the ones distributing benefits. PBMs get in the middle of care decisions that should be made between a patient and their doctor.
Medicine utilization management tactics like prior authorization—which involves restricting a person’s access to a medicines before the insurer approves, even with a doctor’s approval—can lead patients to cut doses in half, skip doses, or adopt other cost-saving measures that may put their health at risk.
Patient Insight #3:
Unexpected healthcare events create barriers to entry
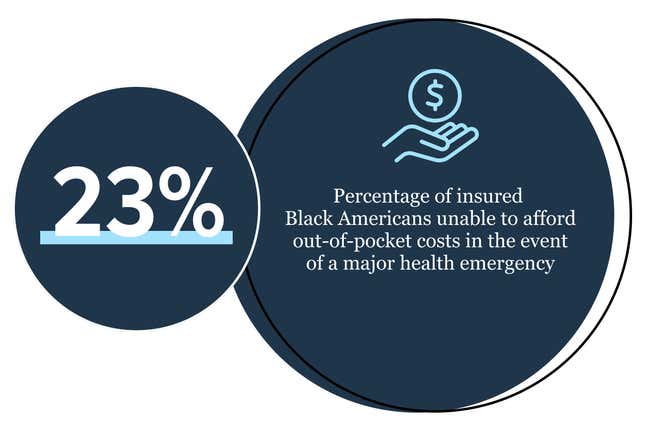
In theory, health insurance coverage should give Americans peace of mind so they know they can access health care when they need it, whether due to an unanticipated acute health condition, hospitalization, or a new diagnosis. But, in practice, Americans’ current healthcare coverage just isn’t doing that job, according to the Patient Experience Survey.
Out of the insured Black Americans surveyed, 23% report that if they encountered a major unforeseen healthcare diagnosis, their out-of-pocket costs would be more than they could afford. Compare this statistic with the fact that though Black Americans represent 14.2% of the population, they are more likely to die from heart disease each year as compared to other racial and ethnic groups. In fact, they are up to two times more likely to die from the leading cause of death in the United States as compared to other racial and ethnic subgroups.
When it comes to reforming the healthcare system, Americans appear to be united on what they want to see from insurance companies and medical providers. For instance, 93% of patients surveyed by PhRMA agreed that doctors—rather than PBMs—should be the final determiners of whether or not a specific medicine is appropriate. Additionally, 88% of participants believe it is wrong that they pay more for their medicine out of pocket than their insurance company or PBM.
Across the board, patients are calling for lower out-of-pocket costs, more equitable cost-sharing with their insurer, and greater transparency at clinics and hospitals. This would facilitate greater medical accessibility and reduce mental and financial stress on all American populations, especially among those of us who are most vulnerable.
Dig into more of the findings in PhRMA’s new Patient Experience Survey.
This post is a sponsored collaboration between PhRMA and G/O Media Studios.

